Browse Articles
Editorial
Vinod B. Shidham, Martha B. Pitman, Richard M. DeMay, Barbara F. Atkinson
Case Report
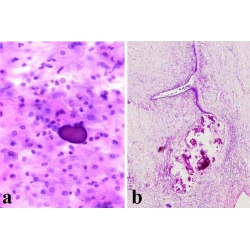
Deepali Jain, Nita Khurana, Shyama Jain
Book Review
Melina Flanagan, Prabodh Gupta
Case Report
Bo Jian, Ana S. Kolansky, Zubair W. Baloach, Prabodh K. Gupta
Book Review
Prabodh K Gupta
Research
Michael J Thrall, Donna K Russell, Thomas A Bonfiglio, Rana S Hoda
Research
Sanjib Kumar Pattari, Pranab Dey, Subhash K Gupta, Kusum Joshi
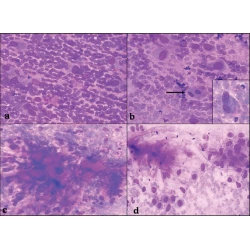
Case Report
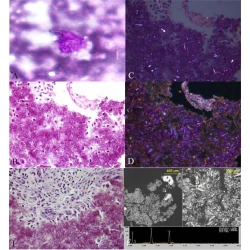
Asghar H Naqvi, Jerrold L Abraham, Robert M Kellman, Kamal K Khurana
Research
Teresa Pusiol, Anna M Parolari, Irene Piscioli, Luca Morelli, Franca Del Nonno, Stefano Licci
Review
Zubair W Baloch, Edmund S Cibas, Douglas P Clark, Lester J Layfield, Britt-Marie Ljung, Martha Bishop Pitman, Andrea Abati
Case Report
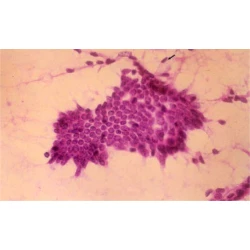
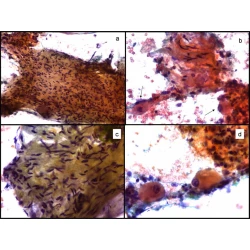
Marco A Ponce-Camacho, Ricardo Diaz de Leon-Medina, Ivett Miranda-Maldonado, Raquel Garza-Guajardo, Jorge Hernandez-Salazar, Oralia Barboza-Quintana
Research
Husain A Saleh, Lewis Clayman, Haitham Masri
Research
Husain A Saleh, Jamal Hammoud, Richard Zakaria, Aurang Zeb Khan
Case Report
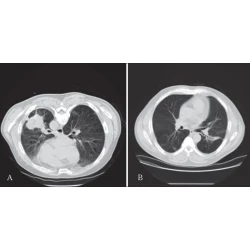
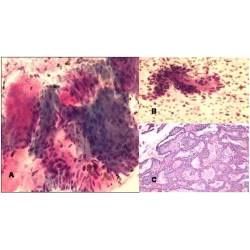
Giancarlo Troncone, Maria Russo, Umberto Malapelle, Marina Accardo, Angelo Ferraro, Immacolata Cozzolino, Lucio Palombini
Research
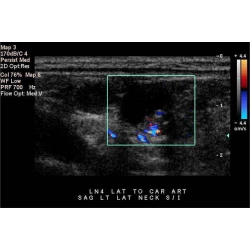
Zubair W Baloch, Julieta E Barroeta, Janet Walsh, Prabodh K Gupta, Virginia A Livolsi, Jill E Langer, Susan J Mandel